- Newsletter
Antiepileptic Drugs Classification
A Comprehensive Exploration of Antiepileptic Drug Classification: Mechanism of Action, Examples, and Clinical Applications
Epilepsy, a neurological disorder characterized by recurrent seizures, affects millions of individuals worldwide. Antiepileptic drugs (AEDs) are the cornerstone of epilepsy management, playing a crucial role in controlling seizures and improving the quality of life for those living with the condition. In this in-depth article, we will take a comprehensive dive into the classification of AEDs, their intricate mechanisms of action, and their specific clinical applications, offering a deeper understanding for healthcare professionals and individuals affected by epilepsy.
Antiepileptic Drugs Classification
Antiepileptic drugs encompass a broad range of medications, which can be classified into several categories based on their mechanism of action. These categories include:
1. Voltage-Gated Sodium Channel Blockers
Sodium channel blockers, such as phenytoin, carbamazepine, and lamotrigine, act by inhibiting the influx of sodium ions into neurons during the depolarization phase. By doing so, they reduce the excitability of hyperactive neurons and help prevent the spread of abnormal electrical activity, thereby controlling seizures. These drugs are primarily used in the treatment of focal seizures, but some can also be effective against generalized seizures.
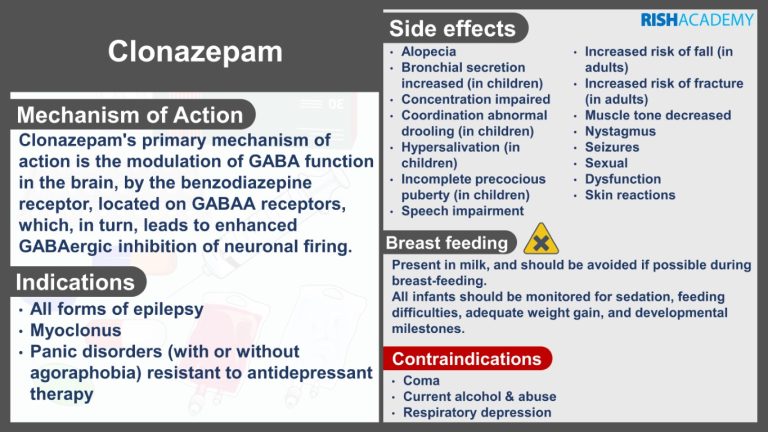
2. GABAergic Drugs
Gamma-aminobutyric acid (GABA) is the primary inhibitory neurotransmitter in the central nervous system. GABAergic drugs enhance GABA-mediated inhibitory signaling, thereby reducing neuronal excitability and dampening seizure activity. This category includes benzodiazepines (e.g., diazepam, clonazepam), barbiturates (e.g., phenobarbital), and certain AEDs, such as valproate and tiagabine. These drugs are employed in the management of various seizure types, including generalized tonic-clonic seizures and absence seizures.
3. Calcium Channel Modulators
Calcium channel modulators, like ethosuximide, act by blocking T-type calcium channels in the thalamus. This mechanism helps to regulate the abnormal burst firing of thalamic neurons associated with absence seizures, making ethosuximide a specific choice for treating this seizure type.
4. Glutamate Antagonists
Glutamate is the major excitatory neurotransmitter in the brain, and excessive glutamate activity can contribute to seizure generation. Glutamate antagonists, such as topiramate, felbamate, and perampanel, block glutamate receptors or modulate their function, reducing neuronal excitability and preventing the spread of seizures. These drugs are utilized in the treatment of both focal and generalized seizures.
5. Other Mechanisms of Action
Some AEDs exhibit unique mechanisms of action that do not fit into the aforementioned categories. For example, valproate exerts its antiepileptic effects through multiple mechanisms, including sodium channel blockade, enhancement of GABA activity, and inhibition of certain enzymes involved in neurotransmitter metabolism. Valproate has a broad-spectrum of activity and is effective in treating various seizure types.
Clinical Applications of Antiepileptic Drugs
The selection of an appropriate AED depends on several factors, including the type of seizures, the patient’s age, comorbidities, and potential drug interactions. Here are some specific clinical applications of commonly used AEDs:
1. Phenytoin
Phenytoin is a first-line treatment for focal seizures and generalized tonic-clonic seizures. Its mechanism of action involves sodium channel blockade, which stabilizes neuronal membranes and prevents abnormal electrical activity.
2. Valproate
Valproate is a versatile AED used to treat absence seizures, focal seizures, generalized tonic-clonic seizures, and myoclonic seizures. Its multiple mechanisms of action, including sodium channel blockade and enhancement of GABA activity, contribute to its broad-spectrum efficacy.
3. Lamotrigine
Lamotrigine is primarily indicated for focal seizures, but it can also be effective against generalized seizures. It acts by inhibiting voltage-gated sodium channels and modulating glutamate release, reducing excitability and dampening seizure activity.
4. Levetiracetam
Levetiracetam is a broad-spectrum AED employed in the management of focal seizures and myoclonic seizures. Although its precise mechanism of action is not fully elucidated, it is thought to modulate neurotransmitter release and inhibit calcium channels.
5. Ethosuximide
Ethosuximide specifically targets absence seizures by blocking T-type calcium channels in the thalamus, which helps normalize the abnormal thalamic rhythmicity associated with this seizure type.
Conclusion
A thorough understanding of antiepileptic drugs classification, their intricate mechanisms of action, and specific clinical applications is paramount in effectively managing epilepsy. By tailoring treatment plans to the seizure type, individual patient characteristics, and potential drug interactions, healthcare professionals can optimize seizure control and enhance the overall quality of life for individuals living with epilepsy. Continued research and advancements in AEDs hold promise for further improving epilepsy management and reducing the burden of this neurological disorder.
- Library