- Newsletter
Classification of Anti Diabetic Drugs
Classification of Anti-Diabetic Drugs
Classification of Anti Diabetic Drugs is important in understanding the mechanism of action of antidiabetic drugs.
There are two different types of diabetes: type 1 diabetes and type 2 diabetes. Lack of insulin is the underlying cause of type 1 diabetes.
In type 1 diabetes, insulin must be administered by injection.
In type 2 diabetes, Insulin resistance in cells is the underlying cause. The most common type of diabetes is type 2.
Both types of diabetics require medication to keep maintain normal blood sugar levels. Depending on the type of diabetes you have, different medicines are used. The categories of antidiabetic medications and their mode of action are discussed in this article.
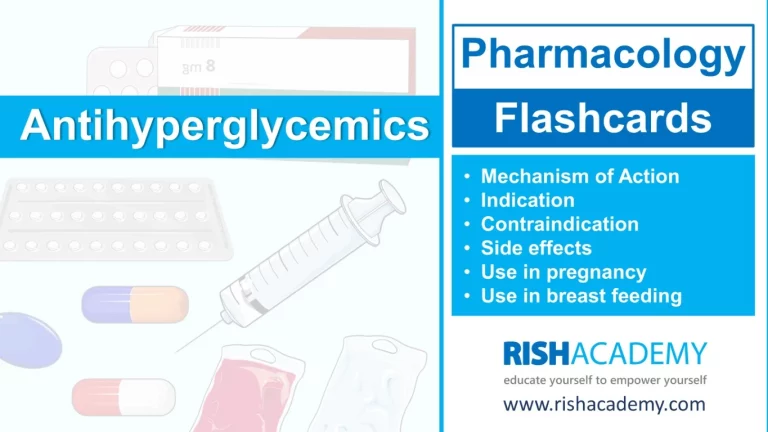
1) Biguanides
Mechanism of action : Biguanides reduce hepatic glucose output and increase the uptake of glucose by the periphery, including skeletal muscle.
Metformin, a biguanide, has become the most commonly used medicine for type 2 diabetes in children and teenagers, although it must be used with caution in patients with impaired liver or kidney function. Metformin is usually the first-line medication used for the treatment of type 2 diabetes. Among common diabetic drugs, Metformin is the only widely used oral drug that does not cause weight gain.
Metformin (Glucophage) may be the best choice for patients who also have heart failure, but it should be temporarily discontinued before any radiographic procedure involving intravenous iodinated contrast, as patients are at an increased risk of lactic acidosis.
2) Thiazolidinediones
Mechanism of action : Reduce insulin resistance through the stimulation of PPARs (peroxisome proliferator-activated receptors). These PPARs act on peroxisome proliferator responsive elements (PPRE). The PPREs influence insulin-sensitive genes, which enhance production of mRNAs of insulin-dependent enzymes. The final result is a better use of glucose by the cells.
Some Examples are : Rosiglitazone, Pioglitazone, Troglitazone
3) Glycosurics / SGLT-2 Inhibitors
Mechanism of action : Glycosurics, also known as SGLT-2 inhibitors, are medications used for treating type 2 diabetes. They work by blocking a protein called SGLT-2 in the kidneys, which leads to increased excretion of glucose in the urine. This helps lower blood glucose levels and improve glycemic control. Additionally, they may have mild diuretic effects and contribute to reducing blood pressure.
Examples : Empagliflozin, Dapagliflozin, Canagliflozin, Remogliflozin
4) Alpha-glucosidase inhibitors
Mechanism of action : Alpha-glucosidase inhibitors work by blocking the enzymes in the small intestine that break down carbohydrates into glucose. By inhibiting these enzymes, they slow down the absorption of carbohydrates and help control post-meal blood sugar spikes.
Some Examples are : Acarbose, Miglitol, Voglibose
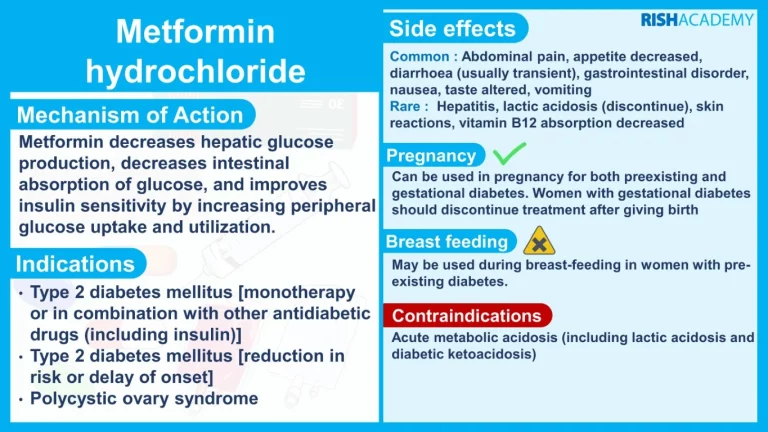
5) Sulfonylureas
Mechanism of action : Sulfonylureas increase insulin secretion from pancreatic β-cells. They are insulin secretagogues, triggering insulin release by inhibiting the KATP channel of the pancreatic beta cells.
First generation Sulfonylureas : Tolbutamide, Tolazamide, Chlorpropamide
Second-generation Sulfonylureas : Gliclazide, Glipizide, Glyburide or Glibenclamide, Glimepiride, Glyclopyramide, Gliquidone
6) Meglitinides
Mechanism of action : Meglitinides help the pancreas produce insulin and are often called “short-acting secretagogues.” They act on the same potassium channels as sulfonylureas but at a different binding site. By closing the potassium channels of the pancreatic beta cells, they open the calcium channels, thereby enhancing insulin secretion.
Examples : Repaglinide, Nateglinide
7) Dipeptidyl peptidase-4 inhibitors
Mechanism of action : They work by blocking the action of an enzyme called DPP-4, which breaks down hormones involved in glucose regulation. By inhibiting DPP-4, these medications increase the levels of these hormones, leading to enhanced insulin secretion, reduced glucagon secretion, and improved blood sugar control.
Examples : Sitagliptin, Vildagliptin, Saxagliptin, Linagliptin, Alogliptin, Septagliptin, Teneligliptin, Gemigliptin
8) Insulin
Typically, insulin is administered subcutaneously either injections or an insulin pump. Insulin may also be infused intravenously in situations that would provide acute care.
Rapid-acting insulins (peak at ~1 hour) are:
- Insulin lispro
- Insulin aspart
- Insulin glulisine
Short-acting insulins (peak 2–4 hours) are:
- Regular insulin (Humulin R, Novolin R)
- Prompt insulin zinc (Semilente)
Intermediate-acting insulins (peak 4–10 hours) are:
- Isophane insulin, neutral protamine Hagedorn (NPH) (Humulin N, Novolin N)
- Insulin zinc (Lente)
Long-acting insulins (duration 24 hours, often without peak) are:
- Extended insulin zinc insulin (Ultralente)
- Insulin glargine (Lantus)
- Insulin detemir (Levemir)
- Insulin degludec (Tresiba)
- Library