- Newsletter
Mechanism of Action of All Drugs
This is a pretty comprehensive article that explains the mechanism of action of all commonly prescribed medications.
1. Analgesics
Paracetamol (Acetaminophen) Mechanism of Action
Weak inhibitor of the synthesis of prostaglandins, Paracetamol also decreases prostaglandin concentrations in vivo.
Aspirin Mechanism of Action
Aspirin causes reduction of inflammation, analgesia, the prevention of clotting, and antipyretic. Much of this is believed to be due to decreased production of prostaglandins and thromboxane A2 by its irreversible inactivation of the cyclooxygenase (COX) enzyme, Cyclooxygenase is required for prostaglandin and thromboxane synthesis.
Diclofenac Sodium Mechanism of Action
Diclofenac has analgesic, anti-inflammatory, and antipyretic properties. It causes inhibition of cyclooxygenase (COX 1 and COX 2) and acts as a potent inhibitor of prostaglandin synthesis in vitro.
Tramadol hydrochloride Mechanism of Action
Tramadol acts on the mu-opioid receptor, blocking the neuron from communicating pain to the brain.
Pethidine hydrochloride (Meperidine) Mechanism of Action
Pethidine exerts its analgesic effects by acting as an agonist at the μ opioid receptor
Morphine Mechanism of Action
Morphine is an Opioid analgesic, activating opiate receptors that are widely distributed throughout the brain and body. Once an opiate reaches the brain, it quickly activates the opiate receptors that are found in many brain regions & produce pleasure (or reward) and pain relief. The brain itself also produces substances known as endorphins that activate the opiate receptors. Morphine mimics endogenous neurotransmitters (endorphins). Morphine binds to specific morphine-like (endorphin) receptors ( EndR).
2. Antiarrhythmics
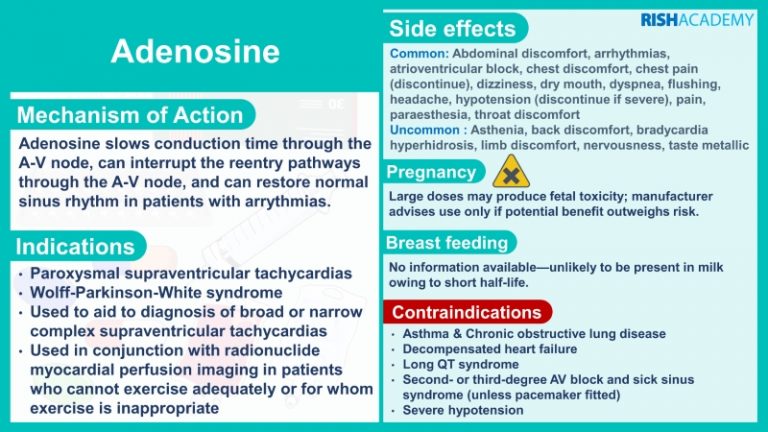
Adenosine Mechanism of Action
Adenosine slows conduction time through the AV node, can interrupt the reentry pathways through the AV node, and can restore normal sinus rhythm in patients with arrhythmias.
Amiodarone hydrochloride Mechanism of Action
It’s primarily a class III antiarrhythmic. Like other antiarrhythmic drugs of this class, amiodarone works primarily by blocking potassium rectifier currents that are responsible for the repolarization of the heart during phase 3 of the cardiac action potential.
Digoxin Mechanism of Action
Digoxin increases the force of contraction of the heart muscles by inhibiting the activity of an enzyme (ATPase) that controls the movement of calcium, sodium, and potassium into the heart muscle. Inhibiting ATPase increases calcium in heart muscle and therefore increases the force of heart contractions. Digoxin also slows electrical conduction between the atria and the ventricles of the heart and is useful in treating arrhythmias.
Bisoprolol fumarate Mechanism of Action
Bisoprolol is a synthetic beta1 selective beta-adrenergic receptor blocker with a low affinity for beta2 receptors in bronchial smooth muscle, blood vessels, and fat cells and no intrinsic sympathomimetic activity. Therefore Bisoprolol exerts cardioselective effects include lower heart rate, decreased cardiac output, and inhibition of renin release by kidneys. At higher doses, it will lose beta1 selectivity.
Atenolol Mechanism of Action
It’s a Cardioselective beta 1 adrenergic antagonist, works by selectively binding to the beta 1 adrenergic receptors found in vascular smooth muscle and the heart, blocking the positive inotropic and chronotropic actions of endogenous catecholamines, thereby inhibiting sympathetic stimulation. This activity results in a reduction in heart rate, blood pressure, and decreases myocardial contractility.
Diltiazem hydrochloride Mechanism of Action
Diltiazem is a benzothiazepine derivative with antihypertensive, antiarrhythmic properties. It blocks voltage-sensitive calcium channels in the blood vessels, by inhibiting the ion control gating mechanisms, thereby preventing calcium levels from increase
3. Antibiotics
Amoxicillin Mechanism of Action
Amoxicillin is in the class of beta-lactam antibiotics. Beta lactams act by binding to penicillin-binding proteins that inhibit a process called transpeptidation, leading to activation of autolytic enzymes in the bacterial cell wall. This process leads to lysis of the cell wall, and thus, the destruction of the bacterial cell. This type of activity is referred to as bactericidal killing.
Azithromycin Mechanism of Action
Azithromycin prevents bacteria from growing by interfering with their protein synthesis. It binds to the 50S subunit of the bacterial ribosome, thus inhibiting the translation of mRNA.
Cefuroxime Mechanism of Action
It’s a Cephalosporin group antibiotic, exerts bactericidal activity by interfering with bacterial cell wall synthesis and inhibiting cross-linking of the peptidoglycan. The cephalosporins are also thought to play a role in the activation of bacterial cell autolysins which may contribute to bacterial cell lysis.
Cephalexin (Cefalexin) Mechanism of Action
It’s a Cephalosporin group antibiotic, exerts bactericidal activity by interfering with bacterial cell wall synthesis and inhibiting cross-linking of the peptidoglycan. The cephalosporins are also thought to play a role in the activation of bacterial cell autolysins which may contribute to bacterial cell lysis.
Ciprofloxacin Mechanism of Action
Ciprofloxacin is a bactericidal antibiotic of the fluoroquinolone drug class. It acts on bacterial topoisomerase II (DNA gyrase) and topoisomerase IV. Ciprofloxacin’s targeting of the alpha subunits of DNA gyrase prevents it from supercoiling the bacterial DNA which prevents DNA replication.
Clarithromycin Mechanism of Action
Clarithromycin, a macrolide antibiotic, inhibits bacterial protein synthesis by binding to the bacterial 50S ribosomal subunit. Binding inhibits peptidyl transferase activity and interferes with amino acid translocation during the translation and protein assembly process, and prevents bacterial protein synthesis.
Clindamycin Mechanism of Action
It is a bacterial protein synthesis inhibitor by inhibiting ribosomal translocation in a similar way to macrolides. It does so by binding to the 23S RNA of the 50S subunit of the ribosome. Clindamycin is bacteriostatic.
Co-amoxiclav Mechanism of Action
Co-amoxiclav is a combination of Amoxicillin and Clavulanic acid. Clavulanic acid blocks the chemical defense, known as beta-lactamase, that some bacteria produce against penicillin group antibiotics such as amoxicillin. Co-amoxiclav is active against bacterial infections that have become resistant to amoxicillin.
Co-trimoxazole Mechanism of Action
Co-trimoxazole, generally bactericidal, a combination of trimethoprim and sulfamethoxazole. It acts by sequential blockade of folic acid enzymes in the synthesis pathway. The sulfamethoxazole component inhibits the formation of dihydrofolic acid from para-aminobenzoic (PABA), whereas trimethoprim inhibits dihydrofolate reductase. Both drugs block folic acid synthesis, preventing bacterial cell synthesis of essential nucleic acids.
Doxycycline Mechanism of Action
Doxycycline is a tetracycline group, a broad-spectrum antibiotic. It inhibits the synthesis of bacterial proteins by binding to the 30S ribosomal subunit, which is only found in bacteria. This prevents the binding of transfer RNA to messenger RNA, so new proteins cannot be made. This stops bacterial growth giving the immune system time to kill and remove the bacteria.
Flucloxacillin Mechanism of Action
Like other β lactam antibiotics, flucloxacillin acts by inhibiting the synthesis of bacterial cell walls. It inhibits cross-linkage between the linear peptidoglycan polymer chains that make up a major component of the cell wall of Gram-positive bacteria.
Gentamycin Mechanism of Action
Gentamicin is and Aminoglycoside, “irreversibly” bind to a specific 30S subunit of the ribosome. This leads to interference with the initiation complex, misreading of mRNA so incorrect amino acids are inserted into the polypeptide leading to nonfunctional or toxic peptides and ultimately inhibits bacterial protein synthesis.
Levofloxacin Mechanism of Action
Levofloxacin is a bactericidal antibiotic of the fluoroquinolone drug class. It acts on bacterial topoisomerase II (DNA gyrase) and topoisomerase IV. Levofloxacin’s targeting of the alpha subunits of DNA gyrase prevents it from supercoiling the bacterial DNA which prevents DNA replication.
Meropenem Mechanism of Action
Meropenem is a broad-spectrum carbapenem antibiotic. It inhibits bacterial cell wall synthesis like other β lactam antibiotics, thus it acts by binding to penicillin-binding proteins that inhibit a process called transpeptidation, leading to activation of autolytic enzymes in the bacterial cell wall. This process leads to lysis of the cell wall, and thus, the destruction of the bacterial cell. Meropenem is bactericidal except against Listeria monocytogenes, where it is bacteriostatic.
Metronidazole Mechanism of Action
Metronidazole is of the nitroimidazole class. It inhibits nucleic acid synthesis by disrupting the DNA of microbial cells. They also lead to the production of toxic metabolites, which may damage the DNA of replicating organisms, usually anaerobic bacteria and protozoans
Vancomycin Mechanism of Action
The bactericidal action of vancomycin results from inhibition of cell wall biosynthesis. Vancomycin forms hydrogen bonds & prevents incorporation of N acetylmuramic acid (NAM) and N acetylglucosamine (NAG) peptide subunits from being incorporated into the peptidoglycan matrix, which forms the major structural component of Gram positive cell walls. Additionally, vancomycin alters bacterial cell membrane permeability and RNA synthesis. Vancomycin is not active in vitro against gram-negative bacilli, mycobacteria, or fungi.
4. Anticoagulants
Apixaban Mechanism of Action
Apixaban is a highly selective, orally bioavailable, and reversible direct inhibitor of free and clot bound factor Xa. (Factor Xa catalyzes the conversion of prothrombin to thrombin, the final enzyme in the coagulation cascade that is responsible for fibrin clot formation)
Enoxaparin sodium Mechanism of Action
Enoxaparin binds to and potentiates antithrombin (a circulating anticoagulant) to form a complex that irreversibly inactivates clotting factor Xa
Fondaparinux sodium Mechanism of Action
Fondaparinux is a synthetic pentasaccharide that binds antithrombin and accelerates its inhibition of factor Xa
Heparin Mechanism of Action
Heparin binds to the enzyme inhibitor antithrombin III (AT) by a conformational change. The activated AT then inactivates thrombin, factor Xa, and other proteases. The rate of inactivation of these proteases by AT can increase by up to 1000 fold due to the binding of heparin & prevents clotting
Rivaroxaban Mechanism of Action
Mechanism of action. Rivaroxaban competitively inhibits free and clot bound factor Xa
Warfarin sodium Mechanism of Action
Warfarin decreases blood clotting by blocking an enzyme called vitamin K epoxide reductase that reactivates vitamin K1. Without sufficient active vitamin K1, clotting factors II, VII, IX, and X have decreased clotting ability.
5. Anticonvulsants
Carbamazepine Mechanism of Action
Carbamazepine is a sodium channel blocker. It binds preferentially to voltage-gated sodium channels in their inactive conformation, which prevents repetitive and sustained firing of an action potential.
Clonazepam Mechanism of Action
Clonazepam’s primary mechanism of action is the modulation of GABA function in the brain, by the benzodiazepine receptor, located on GABAA receptors, which, in turn, leads to enhanced GABAergic inhibition of neuronal firing.
Diazepam Mechanism of Action
Diazepam is a Benzodiazepine, It binds to specific receptors in the central nervous system. They thus cause an increased inhibitory effect of the neurotransmitter gamma aminobutyric acid (GABA).
Gabapentin Mechanism of Action
Gabapentin was designed to mimic the neurotransmitter GABA. It does not, however, bind to GABA receptors. Its mechanism of action as an antiepileptic agent likely involves its inhibition of the alpha 2 delta subunit of voltage gated calcium channels
Levetiracetam Mechanism of Action
Levetiracetam is an antiepileptic drug and the action is modulation of synaptic neurotransmitter release through binding to the synaptic vesicle protein SV2A in the brain
Lorazepam Mechanism of Action
Lorazepam is a benzodiazepine with anxiolytic, anti anxiety, anticonvulsant, antiemetic, and sedative properties. Lorazepam enhances the effect of the inhibitory neurotransmitter gamma aminobutyric acid on the GABA receptors by binding to a site that is distinct from the GABA binding site in the central nervous system.
Phenytoin Mechanism of Action
Phenytoin blocks the voltage gated sodium channels in the brain. This blocks sustained high-frequency repetitive firing of action potentials to protect against seizures
Sodium valproate Mechanism of Action
The anticonvulsant effect of Sodium valproate has been attributed to the blockade of voltage-gated sodium channels and increased brain levels of gamma-aminobutyric acid (GABA).
6. Antidepressants
Amitriptyline hydrochloride Mechanism of Action
Amitriptyline is in the tricyclic antidepressant (TCA) drug classification and acts by blocking the reuptake of both
serotonin and norepinephrine neurotransmitters.
Citalopram Mechanism of Action
The mechanism of action of citalopram results from its inhibition of CNS neuronal reuptake of serotonin (5 HT)
Fluoxetine Mechanism of Action
Fluoxetine is a selective serotonin reuptake inhibitor (SSRI) and as the name suggests, it exerts its therapeutic effect by inhibiting the presynaptic reuptake of the neurotransmitter serotonin
Sertraline Mechanism of Action
Sertraline selectively inhibits the reuptake of serotonin (5 HT) at the presynaptic neuronal membrane, thereby increasing serotonergic activity. This results in an increased synaptic concentration of serotonin in the CNS, which leads to numerous functional changes associated with enhanced serotonergic neurotransmission.
Venlafaxine Mechanism of Action
Venlafaxine and its active metabolite, O desmethylvenlafaxine (ODV), inhibit the reuptake of both serotonin and norepinephrine, thus increases the neurotransmitter activity in the brain
7. Antiemetics
Cyclizine Mechanism of Action
Cyclizine is a histamine H1 receptor antagonist of the piperazine class and It possesses antiemetic properties.
Levomepromazine Mechanism of Action
Although the exact mechanism of action of levomepromazine is not fully known, upon administration, this agent appears to act as an antagonist for a variety of receptors in the central nervous system (CNS), including adrenergic, dopamine, histamine, cholinergic, and serotonin (5 hydroxytryptamine; 5 HT) receptors.
Metoclopramide hydrochloride Mechanism of Action
The antiemetic action of metoclopramide is due to its antagonist activity at D2 receptors in the chemoreceptor trigger zone in the central nervous system. This action prevents nausea and vomiting.
Ondansetron Mechanism of Action
Ondansetron is a specific 5HT3 receptor antagonist which blocks 5HT3 receptors in the gastrointestinal tract and in the central nervous system.
Prochlorperazine Mechanism of Action
Prochlorperazine mainly blocks D2 dopamine receptors in the brain. It can also block histaminergic, cholinergic, and noradrenergic receptors.
8. Antihyperglycemics
Gliclazide Mechanism of Action
Gliclazide, a sulfonylurea binds to the β cell sulfonylurea receptor (SUR1). This binding subsequently blocks the ATP-sensitive potassium channels & results in the closure of the channels and leads to a resulting decrease in potassium efflux leads to depolarization of the β cells. This opens voltage-dependent calcium channels in the β cell resulting in calmodulin activation, which in turn leads to exocytosis of insulin-containing secretory granules.
Metformin hydrochloride Mechanism of Action
Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization.
9. Antihypertensives
Amlodipine Mechanism of Action
Amlodipine is an angioselective calcium channel blocker and inhibits the movement of calcium ions into vascular smooth muscle cells and cardiac muscle cells which inhibits the contraction of cardiac muscle and vascular smooth muscle cells
Atenolol Mechanism of Action
It’s a Cardioselective beta 1 adrenergic antagonist, works by selectively binding to the beta 1 adrenergic receptors found in vascular smooth muscle and the heart, blocking the positive inotropic and chronotropic actions of endogenous catecholamines, thereby inhibiting sympathetic stimulation. This activity results in a reduction in heart rate, blood pressure, and decreases myocardial contractility.
Bisoprolol fumarate Mechanism of Action
Bisoprolol is a synthetic beta1 selective beta-adrenergic receptor blocker with a low affinity for beta2 receptors in bronchial smooth muscle, blood vessels, and fat cells and no intrinsic sympathomimetic activity. Therefore Bisoprolol exerts cardio-selective effects include lower heart rate, decreased cardiac output, and inhibition of renin release by kidneys. At higher doses, it will lose beta1 selectivity.
Candesartan cilexetil Mechanism of Action
Candesartan selectively blocks the binding of angiotensin II to AT1 in many tissues including vascular smooth muscle and the adrenal glands. This inhibits the AT1 mediated vasoconstrictive and aldosterone secreting effects of angiotensin II and results in an overall decrease in blood pressure.
Diltiazem hydrochloride Mechanism of Action
Diltiazem is a calcium channel blocker whose mechanism of action is the prevention of forward movement of calcium ions through slow channels in myocardial and vascular smooth muscle cells. It is a negative inotrope and it reduces vascular resistance.
Doxazosin Mechanism of Action
Doxazosin selectively inhibits the postsynaptic alpha 1 receptors on vascular smooth muscle by nonselectively blocking the alpha 1a, alpha 1b, and alpha 1d subtypes12,13. This action on blood vessels decrease systemic peripheral vascular resistance, reducing blood pressure
Lisinopril Mechanism of Action
Lisinopril inhibits angiotensin-converting enzyme (ACE). ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex. By these actions, Lisinopril acts as a vasodilator and reduces blood pressure
Losartan potassium Mechanism of Action
Losartan is a nonpeptide angiotensin II receptor antagonist with high affinity and selectivity for the AT 1 receptor. Losartan blocks the vasoconstrictor and aldosterone secreting effects of angiotensin II by inhibiting the binding of angiotensin II to the AT 1 receptor.
Nifedipine Mechanism of Action
Nifedipine blocks voltage-gated L-type calcium channels in vascular smooth muscle and myocardial cells. This blockage prevents the entry of calcium ions into cells during depolarization, reducing peripheral arterial vascular resistance and dilating coronary arteries. These actions reduce blood pressure and alleviating angina.
Ramipril Mechanism of Action
Ramipril inhibits angiotensin-converting enzyme (ACE). ACE is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex. By these actions, Ramipril acts as a vasodilator and reduces blood pressure.
10. Antivirals
Acyclovir / Aciclovir Mechanism of Action
Acyclovir is converted to its triphosphate form, acyclovir triphosphate (ACV TP), which competitively inhibits viral DNA polymerase, incorporates into and terminates the growing viral DNA chain, and inactivates the viral DNA polymerase.
Oseltamivir Mechanism of Action
Oseltamivir inhibits the neuraminidase enzyme, which is expressed on the viral surface. The enzyme promotes release of virus from infected cells and facilitates viral movement within the respiratory tract.
Zanamivir Mechanism of Action
The action of Zanamivir is via inhibition of influenza virus neuraminidase with the possibility of alteration of virus particle aggregation and release. By binding and inhibiting the neuraminidase protein, the drug renders the influenza virus unable to escape its host cell and infect others.
11. Bronchodilators
Ipratropium bromide Mechanism of Action
Ipratropium bromide is an anticholinergic parasympatholytic ) agent, which blocks the muscarinic receptors of acetylcholine.
Salbutamol Mechanism of Action
It is a short-acting β2 adrenergic receptor agonist which works by causing relaxation of airway smooth muscle.
Theophylline Mechanism of Action
Theophylline relaxes the smooth muscle of the bronchial airways and pulmonary blood vessels and reduces airway responsiveness to histamine, and allergen. Theophylline competitively inhibits type III and type IV phosphodiesterase (PDE), the enzyme responsible for breaking down cyclic AMP in smooth muscle cells, possibly resulting in bronchodilation. Theophylline also binds to the adenosine A2B receptor and blocks adenosine-mediated bronchoconstriction.
Tiotropium Mechanism of Action
Tiotropium bromide is a long-acting muscarinic antagonist (LAMA). Tiotropium is an antagonist of muscarinic receptors M1 to M5. Inhibition of the M3 receptor in the smooth muscle of the lungs leads to relaxation of smooth muscle and bronchodilation.
12. Diuretics
Amiloride hydrochloride Mechanism of Action
Amiloride hydrochloride is a new, orally-administered, potassium-sparing diuretic with mild natriuretic and diuretic properties. Its primary site of action is the distal tubule of the nephron where it selectively blocks sodium transport, thereby inhibiting sodium potassium exchange.
Bendroflumethiazide Mechanism of Action
Bendroflumethiazide is a thiazide diuretic that works by inhibiting Na+/Cl reabsorption at the beginning of the distal convoluted tubule (DCT) in the kidneys. Water is lost as a result of more sodium reaching the collecting ducts.
Bumetanide Mechanism of Action
Bumetanide interferes with renal cAMP and/or inhibits the sodium-potassium ATPase pump. Bumetanide appears to block the active reabsorption of chloride and possibly sodium in the ascending loop of Henle, altering electrolyte transfer in the proximal tubule. This results in excretion of sodium, chloride, and water, and, hence, diuresis.
Furosemide Mechanism of Action
Furosemide, like other loop diuretics, acts by inhibiting the luminal Na K Cl cotransporter in the thick ascending limb of the loop of Henle, by binding to the chloride transport channel, thus causing sodium, chloride, and potassium loss in urine.
Spironolactone Mechanism of Action
Spironolactone competitively inhibits aldosterone dependant sodium-potassium exchange channels in the distal convoluted tubule. This action leads to increased sodium and water excretion, but more potassium retention. The increased excretion of water leads to diuretic and also antihypertensive effects.
13. Intravenous Fluids
Geloplasma/Gelatin Mechanism of Action
The low blood volume in hypovolaemic shock, burns and cardiopulmonary bypass
Glucose Mechanism of Action
Glucose is also known as dextrose is a simple sugar (monosaccharide) that is used to increase the level of blood sugar (glucose) when the level falls too low (hypoglycemia). Glucose in this form increases the level of the blood sugar, so it is a glucose elevating agent
Hartmann’s solution / Ringer’s
Lactate solution / Sodium
Lactate solution Mechanism of Action
Absorption As Compound Sodium Lactate (Hartmann’s) is directly administered to the systemic circulation, the bioavailability (absorption) of the active components is complete (100%). Excretion Excess of calcium is predominantly excreted by the renal system, as in the case of potassium and sodium excretion.
Normal Saline / Sodium Chloride
Normal saline is a crystalloid fluid. Normal saline contains electrolytes (sodium and chloride ions) which dissociates in solution
14. Laxatives
Bisacodyl Mechanism of Action
Bisacodyl works by stimulating enteric nerves to cause peristalsis, mainly on the colon. It is also a contact laxative, increases fluid and salt secretion.
Glycerin/ Glycerol Mechanism of Action
Glycerin suppositories produce laxative action by causing rectal distention, thereby stimulating the urge to defecate; by causing local rectal irritation; and by triggering a hyperosmolar mechanism that draws water into the colon.
Lactulose Mechanism of Action
Lactulose is a synthetic sugar. It breaks down in your large intestine and then draws water into the intestine. This softens your stool, which helps ease constipation. Lactulose also appears to inhibit intestinal ammonia production several mechanisms. Colonic metabolism of lactulose to lactic acid results in acidification of the gut lumen. This favors the conversion of ammonium (NH4) to ammonia (NH3) and the passage of ammonia from tissues into the lumen, thus reduces blood ammonia concentrations.
Macrogol /Polyethylene Glycol (PEG) Mechanism of Action
Macrogol is an osmotically acting laxative, that is an inert substance that passes through the gut without being absorbed into the body. It relieves constipation because it causes water to be retained in the bowel instead of being absorbed into the body.
Senna Mechanism of Action
Senna contains sennosides which acts as a stimulant laxative. It works by irritating and stimulating intestinal cells, producing contractions in intestines, water influx to the intestines and bowel movement.
Sodium Acid Phosphate with Sodium Phosphate Mechanism of Action
Rectal sodium phosphate is a laxative from the saline laxatives class. Its mechanism of action is not well known, but it is believed that the laxative action may result from phosphate ions that are not well absorbed within the small intestine, causing a retention of water and indirectly increasing bowel movements.
Docusate sodium Mechanism of Action
Docusate lowers the surface tension at the oil water interface of the feces, allowing water and lipids to penetrate the stool. This helps to hydrate and soften the fecal material, facilitating natural defecation.
15. Proton Pump Inhibitors & Drugs Used In Acid Peptic Disease
Esomeprazole Mechanism of Action
Esomeprazole is a proton pump inhibitor that suppresses gastric acid secretion by specific inhibition of the H+/K+ ATPase in the gastric parietal cell.
Lansoprazole Mechanism of Action
Its mechanism of action is to selectively inhibit the membrane enzyme H+/K+ ATPase in gastric parietal cells.
Omeprazole Mechanism of Action
Omeprazole is a selective and irreversible proton pump inhibitor. It suppresses stomach acid secretion by specific inhibition of the H+/K+ ATPase system found at the secretory surface of gastric parietal cells.
Ranitidine Mechanism of Action
Ranitidine is a competitive, reversible inhibitor of the action of histamine at the histamine H2 receptors found in gastric parietal cells. This results in decreased gastric acid secretion and gastric volume, and reduced hydrogen ion concentration.
16. Sedatives
Chlordiazepoxide hydrochloride Mechanism of Action
Chlordiazepoxide binds to stereospecific benzodiazepine (BZD) binding sites on GABA A receptor complexes at several sites within the central nervous system, including the limbic system and reticular formation. This results in increased binding of the inhibitory neurotransmitter GABA to the GABA A receptor. The net neuro inhibitory effects result in the observed sedative, hypnotic, anxiolytic, and muscle relaxant properties.
Diazepam Mechanism of Action
Diazepam is a Benzodiazepine, It binds to specific receptors in the central nervous system. They thus cause an increased inhibitory effect of the neurotransmitter gamma-aminobutyric acid (GABA)
Haloperidol Mechanism of Action
The active mechanism of Haloperidol is to block postsynaptic dopamine (D2) receptors in the mesolimbic system of the brain.
Lorazepam Mechanism of Action
Lorazepam is a benzodiazepine with anxiolytic, anti anxiety, anticonvulsant, antiemetic, and sedative properties. Lorazepam enhances the effect of the inhibitory neurotransmitter gamma-aminobutyric acid on the GABA receptors by binding to a site that is distinct from the GABA binding site in the central nervous system.
Midazolam Mechanism of Action
The actions of benzodiazepines such as midazolam are mediated through the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), which is one of the major inhibitory neurotransmitters in the central nervous system. Benzodiazepines bind to the benzodiazepine site on GABA A receptors, which potentiates the effects of GABA. Benzodiazepines increase the activity of GABA, thereby producing a sedating effect, relaxing skeletal muscles, and inducing sleep, anesthesia, and amnesia.
Phenobarbital (Phenobarbitone) Mechanism of Action
Phenobarbital works by increasing the amount of time chloride channels are open which in turn depresses the central nervous system. This is done by acting on GABA A receptor subunits
Zopiclone Mechanism of Action
Zopiclone exerts its action by binding on the benzodiazepine receptor complex and modulation of the GABA B receptor chloride channel macromolecular complex and causes an enhancement of the inhibitory actions of GABA to produce hypnotic and anxiolytic effects
17. Statins
Atorvastatin Mechanism of Action
Atorvastatin is a statin medication and a competitive inhibitor of the enzyme HMG CoA (3 hydroxy 3 methyl glutaryl coenzyme A) reductase, which catalyzes the
conversion of HMG CoA to mevalonate, an early rate limiting step in cholesterol biosynthesis. Atorvastatin acts primarily in the liver, where decreased hepatic cholesterol concentrations stimulate the upregulation of hepatic low-density lipoprotein (LDL) receptors, which increases hepatic uptake of LDL and lowers plasma
cholesterol levels.
Simvastatin Mechanism of Action
Simvastatin is a statin medication and a competitive inhibitor of the enzyme HMG CoA (3 hydroxy 3 methyl glutaryl coenzyme A) reductase, which catalyzes the conversion of HMG CoA to mevalonate, an early rate-limiting step in cholesterol biosynthesis. Simvastatin acts primarily in the liver, where decreased hepatic cholesterol concentrations stimulate the upregulation of hepatic low-density lipoprotein (LDL) receptors, which increases hepatic uptake of LDL and lowers plasma cholesterol levels.

- Library